Respiratory Depression from Opioids and Other Medications: Critical Signs You Can't Ignore
 Dec, 1 2025
Dec, 1 2025
Opioid Risk Assessment Tool
Assess Your Risk
This tool estimates your risk of respiratory depression based on factors discussed in the article.
When someone takes an opioid for pain, most people assume the worst that can happen is drowsiness or nausea. But the real danger isn’t always obvious - it’s silent. Respiratory depression from opioids and other medications can kill without warning, often before anyone realizes something’s wrong. It doesn’t always look like an overdose. Sometimes, it’s just a person who’s unusually quiet, breathing too slowly, or not waking up when they should. And it’s happening more than you think.
What Exactly Is Respiratory Depression?
Respiratory depression isn’t just slow breathing. It’s when your brain stops telling your lungs to work properly. Opioids bind to receptors in the brainstem - the part that controls automatic functions like breathing - and shut down the signal. The result? Fewer breaths per minute, shallow breaths, and eventually, not enough oxygen getting to your organs.
Doctors define it clinically as fewer than 8 to 10 breaths per minute, paired with oxygen levels dropping below 85%. But here’s the tricky part: if someone is on supplemental oxygen, their oxygen numbers might look fine even while carbon dioxide builds up to dangerous levels. That’s why just checking oxygen saturation isn’t enough. You need to watch the rhythm, depth, and frequency of breathing - not just the number on a monitor.
The Silent Signs: What to Look For
Most people think of respiratory depression as someone gasping or turning blue. In reality, it often starts quietly. Here’s what you’ll actually see in early stages:
- Breathing fewer than 10 times per minute - slower than normal, but not always obviously abnormal
- Shallow breaths that don’t seem to fill the lungs
- Unusual drowsiness - not just tired, but hard to wake up, even with loud noises or shaking
- Confusion or disorientation - acting out of character, unable to answer simple questions
- Lethargy so severe the person doesn’t respond to pain or touch
- Nausea or vomiting - present in over 65% of confirmed cases
- Headache or dizziness - often ignored as side effects, not warning signs
Some people develop a fast heart rate (tachycardia) as the body tries to compensate. Others become cold and clammy. These aren’t random symptoms - they’re your body’s last-ditch effort to stay alive before the system shuts down.
Who’s Most at Risk?
It’s not just people using opioids illegally. Even patients prescribed opioids for surgery or chronic pain are at risk - especially if they have certain factors:
- Age over 60 - risk triples
- Female - women have a 70% higher risk than men
- Never used opioids before - opioid-naïve patients are nearly five times more likely to develop respiratory depression
- Taking other CNS depressants - benzodiazepines (like Xanax or Valium), alcohol, sleep aids, or muscle relaxants
- Multiple health conditions - each additional illness (like COPD, heart failure, or kidney disease) raises risk by almost 3 times
The worst combination? Opioids plus benzodiazepines. This pairing increases the chance of respiratory depression by nearly 15 times. That’s why many hospitals now require pharmacists to review all medications before opioid doses are given.
Why Monitoring Isn’t Enough - And What Actually Works
Most hospitals check vital signs every 4 hours. That means a patient is unmonitored 96% of the time. In that gap, someone can go from breathing normally to stopping breathing entirely.
Here’s what’s proven to save lives:
- Continuous pulse oximetry - for patients not on oxygen, alarms set at 90% saturation or lower
- Capnography - measures carbon dioxide levels. This is critical for patients on supplemental oxygen, since it catches danger before oxygen drops. Capnography is 94% accurate at detecting respiratory depression.
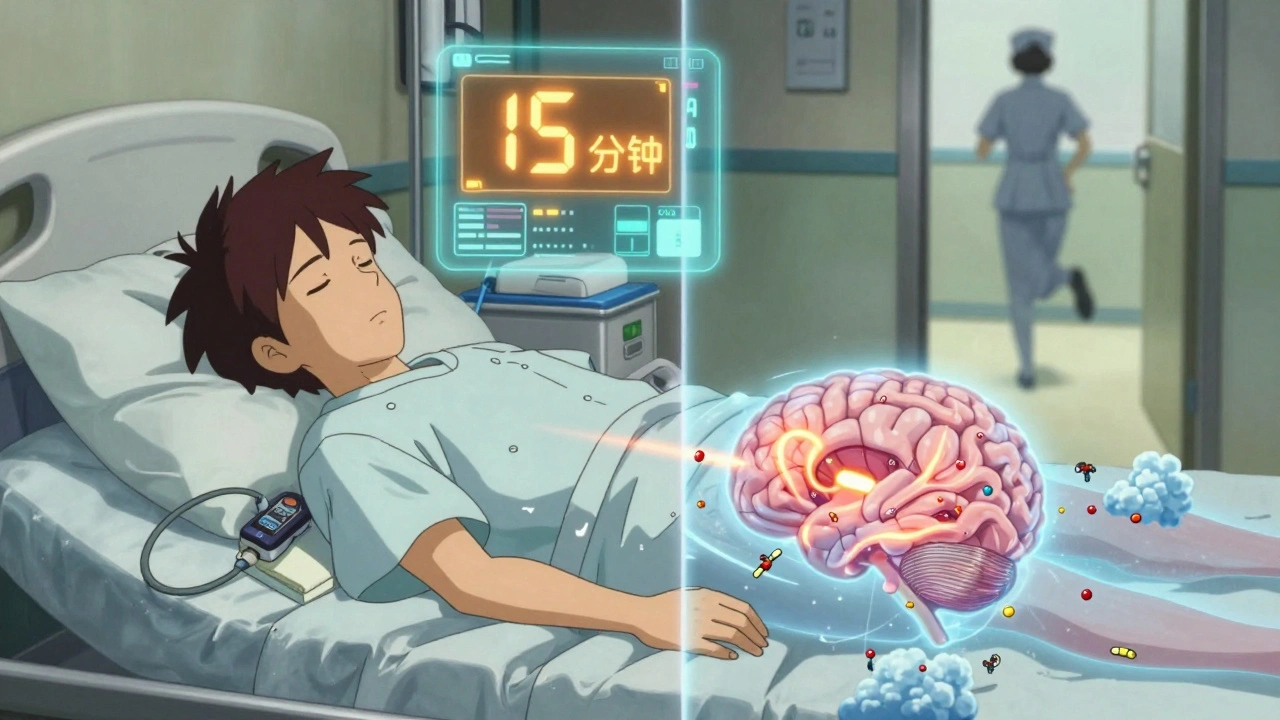
- Real-time alert systems - newer devices combine oximetry, capnography, and motion sensors to predict respiratory depression up to 15 minutes before it becomes obvious. These systems are now used in top hospitals and have cut OIRD events by nearly half.
- Staff training - only 42% of nurses can correctly identify early signs in simulation tests. Training isn’t optional - it’s life-or-death.
Even with good tech, alarm fatigue is a real problem. If alarms go off too often and most are false, staff start ignoring them. That’s why smart systems now prioritize alerts based on actual risk - not just numbers.
What Happens If It’s Not Caught?
Untreated respiratory depression leads to hypoxia - your brain and organs aren’t getting oxygen. After just a few minutes, brain cells begin to die. Permanent damage can happen in under 10 minutes. Death follows quickly after.
And it’s preventable. The Centers for Medicare & Medicaid Services (CMS) now classifies severe respiratory depression from opioids as a “never event” - meaning if it happens in a hospital, they don’t get paid for the extra care needed. That’s how serious it is.
What to Do If You Suspect It
If you’re caring for someone on opioids and notice any of the signs above:
- Try to wake them - shake their shoulder, call their name loudly
- Count their breaths for 15 seconds - multiply by 4. If it’s under 10, act immediately
- Call for emergency help - don’t wait
- If you have naloxone (Narcan), administer it right away - even if you’re not sure
Naloxone reverses opioid effects in minutes. It’s safe to use even if opioids aren’t the cause - it won’t hurt someone who doesn’t need it. But it’s not a cure-all. It wears off faster than some long-acting opioids, so the person can slip back into respiratory depression after the naloxone wears off. That’s why emergency care is mandatory.
How Hospitals Are Fighting Back
Some hospitals have cut respiratory depression cases by 47% using three simple strategies:
- Pharmacist-led opioid dosing - no more automatic prescriptions
- Continuous monitoring for high-risk patients - anyone with two or more risk factors
- Staff training every 6 months - not a one-time lecture, but hands-on simulations
Yet only 22% of U.S. hospitals follow all recommended safety protocols. Community hospitals are far behind academic centers. If your loved one is being treated in a smaller hospital, ask: “Are they using continuous monitoring?” If the answer is no, push for it.
The Future: Safer Opioids and AI Predictions
Scientists are working on new opioids that relieve pain without slowing breathing. One type, called biased mu-opioid receptor agonists, is in late-stage trials. Early results show pain relief with minimal respiratory impact.
Meanwhile, the FDA-approved Opioid Risk Calculator, launched in January 2023, uses 12 factors - age, weight, kidney function, other meds, history of sleep apnea - to predict an individual’s risk with 84% accuracy. It’s not perfect, but it’s a big step toward personalized safety.
AI-powered systems are now being tested to predict breathing problems before they happen. One study showed a system predicting respiratory depression 15 minutes in advance by analyzing tiny changes in breathing patterns, heart rate variability, and movement. These tools could soon be standard in every ICU and post-op unit.
Final Reality Check
Respiratory depression from opioids and other sedatives isn’t rare. It’s common - and often missed. The numbers don’t lie: up to 20,000 Americans need naloxone every year just to survive after a preventable breathing stoppage. Many of those cases happen in hospitals, not on the streets.
You don’t need to be a doctor to save a life. Learn the signs. Know the risk factors. Ask questions. If someone you care about is on opioids - whether it’s for surgery, cancer pain, or chronic back issues - don’t assume they’re safe just because they’re in a hospital. Monitor them. Speak up. Your vigilance might be the only thing between them and a preventable death.

Ella van Rij
December 3, 2025 AT 05:01Oh wow, another ‘wake up sheeple’ post about opioids. Let me grab my monocle and sigh dramatically. I’m sure the 17th hospital nurse reading this is just weeping into her stethoscope because she didn’t know shallow breathing = death. 🙄
Rebecca M.
December 3, 2025 AT 23:25My aunt took oxycodone after knee surgery and slept for 36 hours straight. We thought she was just ‘resting.’ Turns out, her oxygen dipped to 82%. They had to use Narcan. Now she’s on gabapentin and won’t shut up about how ‘the system failed her.’
Lynn Steiner
December 5, 2025 AT 21:09THIS IS WHY I HATE AMERICA. 🇺🇸 People get prescribed opioids like they’re gummy vitamins. My cousin died in a nursing home because they didn’t check her breathing. No one cared. I cried for three days. 😭
Elizabeth Grace
December 7, 2025 AT 01:05My dad’s on long-term opioids for spinal stenosis. I started counting his breaths at night. He’s 72, on Xanax, and has COPD. I used to think he was just ‘sleeping deep.’ Now I have a little notebook. If he’s under 9 breaths, I nudge him. He hates it. But I’d rather be annoying than bury him.
Steve Enck
December 7, 2025 AT 17:18One must consider the epistemological framework underpinning the clinical recognition of respiratory depression. The reductionist reliance on numerical thresholds (e.g., 8–10 breaths/min) ignores the phenomenological experience of the patient’s respiratory rhythm, which is inherently non-linear and context-dependent. Furthermore, the commodification of medical surveillance technologies-capnography, pulse oximetry-represents a neoliberal co-optation of care, wherein algorithmic vigilance replaces human attentiveness. The real tragedy is not the physiological collapse, but the institutional abandonment of embodied presence.
Roger Leiton
December 8, 2025 AT 11:43So true. I work in ER and we had a guy come in last week-prescribed fentanyl patch, took an extra one because he ‘felt tired.’ Oxygen was 94%, but his CO2 was 82. Capnography saved him. 🤯 Also, Narcan is basically magic. I keep a kit in my car now. If you’re around someone on pain meds, learn this. It’s not dramatic-it’s just common sense. 💙
Laura Baur
December 8, 2025 AT 20:31It is both statistically and ethically indefensible that 78% of U.S. hospitals do not implement continuous capnography for opioid-naïve patients, particularly when the marginal cost of such monitoring is less than $200 per device annually. The failure to standardize this protocol constitutes a systemic violation of the non-maleficence principle in medical ethics. Moreover, the conflation of ‘drowsiness’ with ‘safe sedation’ is a dangerous linguistic artifact of medical paternalism. We must demand, as a matter of moral urgency, the institutional adoption of AI-driven predictive analytics-not as a luxury, but as a baseline standard of care. The data is unequivocal. The inaction is criminal.
Jack Dao
December 9, 2025 AT 16:11Of course, the author ignores that 90% of these cases happen because people mix opioids with alcohol. You know, the stuff that’s legal, socially acceptable, and drunk by 70% of Americans on Friday nights. So… blame the drug? Or blame the culture that thinks ‘one more drink’ is fine? 🤔
dave nevogt
December 9, 2025 AT 20:24I’ve sat with my mom during chemo, holding her hand as she drifted off after her pain meds. I didn’t know what to watch for. I just knew she looked peaceful. Now I realize-peaceful isn’t always safe. I wish someone had told me to count breaths. Not because I’m scared, but because I loved her. And I didn’t want to lose her to something silent. I’m glad this post exists. Maybe someone else won’t have to learn the hard way.
Arun kumar
December 10, 2025 AT 02:51in india we dont have much of this problem because doctors dont just give opioids like candy. also naloxone? we dont even have it in most rural hospitals. but we do have strong family watching. if uncle stops breathing, we slap him. works 70% time 😅
Zed theMartian
December 10, 2025 AT 22:33Oh please. This is just Big Pharma’s fear-mongering campaign to sell more ‘smart monitors.’ You know what actually prevents respiratory depression? Not giving opioids in the first place. Let people suffer. Pain is character-building. Also, AI predicting breathing? Sounds like a Black Mirror episode. 🤖💀