Prevent Vomiting During Pregnancy: Practical Tips and Tricks
 Oct, 10 2025
Oct, 10 2025
Morning Sickness Symptom Tracker
Track Your Symptoms
Select the symptoms you experience most frequently to help identify potential triggers and solutions.
Recommended Actions
Select your symptoms and click "Analyze My Triggers" to see personalized recommendations.
Morning sickness can feel like a nonstop battle, but you don’t have to surrender to the waves of nausea. Below are proven, everyday strategies that many expectant mothers use to keep vomiting at bay.
Quick Takeaways
- Eat small, frequent meals and keep a bland snack handy.
- Ginger in tea, candy, or capsules cuts nausea for most women.
- VitaminB6 (25‑50mg) is a safe, first‑line supplement.
- Stay hydrated-sip water, electrolyte drinks, or herbal teas.
- Acupressure wrist bands or pressure on the P6 point can calm the stomach.
- Identify trigger smells and avoid them whenever possible.
- Seek medical advice if vomiting lasts more than 24hours or you can’t keep fluids down.
What is Morning Sickness?
Morning sickness is a common form of nausea and vomiting that affects up to 80% of pregnant people, usually peaking between weeks6 and12. Despite the name, symptoms can strike at any time of day. The condition is caused by rapid hormonal changes, especially rising levels of human chorionic gonadotropin (hCG) and estrogen, which affect the stomach’s lining and the brain’s vomiting center.
Dietary Fixes That Really Work
What you eat (and when) makes a huge difference. Here are the top food‑based tricks, each backed by clinical observations.
- Small, frequent meals: Aim for 5‑6 mini‑meals a day. A handful of crackers, a banana, or a plain yogurt keep blood sugar stable and reduce stomach irritation.
- Ginger contains gingerol and shogaol, compounds that speed gastric emptying and calm the nausea pathways. Try ginger tea, crystallized ginger, or 250mg ginger capsules 30minutes before meals.
- VitaminB6 (pyridoxine) has been shown in multiple trials to cut nausea frequency by about 40%. The usual dose is 25‑50mg three times daily, but always confirm with your provider.
- Cold or room‑temperature foods: Hot, aromatic dishes can intensify smells. Keep foods chilled-think yogurt, cheese sticks, or chilled fruit.
- Protein first: Pair carbs with a protein source (e.g., peanut butter on toast) to slow digestion and avoid spikes that trigger nausea.

Hydration Hacks
Dehydration worsens nausea, yet many women can’t keep liquids down. Try these tricks:
- Sip electrolyte drinks that contain sodium, potassium, and a hint of sugar throughout the day instead of gulping large amounts.
- Freeze water into ice pops flavored with lemon or ginger for a soothing, slow‑release source of fluid.
- Avoid carbonated beverages; the bubbles can expand the stomach and trigger vomit reflexes.
Acupressure, Aromatherapy, and Other Non‑Drug Options
Physical pressure points and scents can modulate the brain’s nausea circuits without medication.
- Acupressure wrist bands apply pressure to the P6 (Neiguan) point located three finger‑widths below the wrist crease. Clinical studies show a 30‑50% reduction in nausea scores when worn consistently.
- Lavender or peppermint essential oil: Inhale from a cotton ball or use a diffuser for short, 5‑minute sessions. Both have modest anti‑nausea effects in small trials.
- Gentle yoga or brisk walking after meals can help gravity move food through the stomach faster.
When Home Remedies Aren’t Enough: Medication Options
If vomiting persists for more than a day, you risk dehydration and weight loss. Your doctor may prescribe one of the following safe anti‑emetic drugs.
| Approach | Typical Onset | Effectiveness (average reduction in nausea episodes) | Safety in Pregnancy |
|---|---|---|---|
| Ginger (250mg) | 30minutes | ~40% | CategoryC - generally considered safe |
| VitaminB6 (25mg) | 1‑2hours | ~35% | CategoryA - safe |
| Doxylamine‑pyridoxine (Diclegis) | 1‑2hours | ~60% | CategoryA - FDA‑approved for nausea |
| Ondansetron (Zofran) | 15‑30minutes | ~70% | CategoryB - used when other options fail |
Always discuss dosage and timing with your obstetrician. Most providers start with vitaminB6 and ginger, then add doxylamine‑pyridoxine if needed. Ondansetron is reserved for severe cases because of a slightly higher, though still low, risk profile.
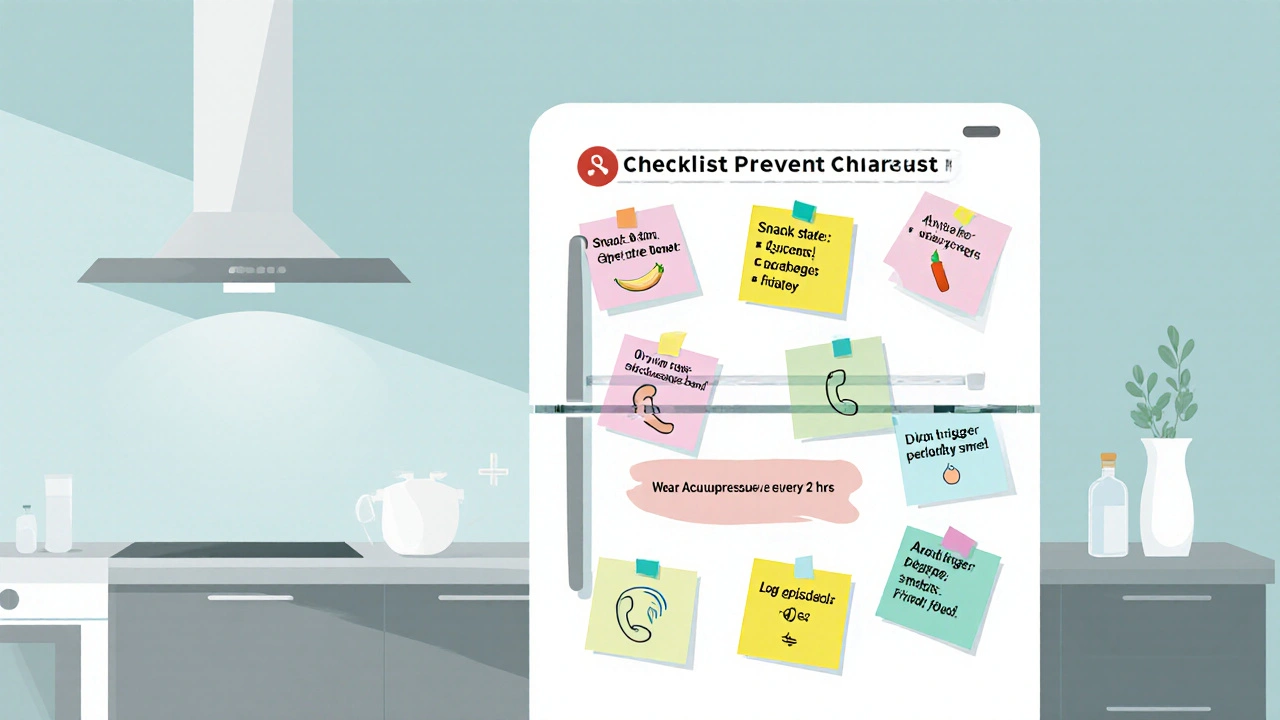
Checklist: Preventing Vomiting Day‑to‑Day
- Set a snack station with crackers, ginger chews, and fruit.
- Drink 8‑10oz of water or electrolyte beverage every two hours.
- Wear acupressure bands from morning until bedtime.
- Keep a list of trigger smells (e.g., perfume, fried foods) and ask family to avoid them.
- Schedule prenatal vitamins with meals, not on an empty stomach.
- Log any episodes of vomiting; bring the log to your next appointment.
When to Call Your Healthcare Provider
While most nausea resolves by the end of the first trimester, watch for these red flags:
- Vomiting more than 3‑4 times in 24hours.
- Inability to keep any fluids down for 24hours.
- Weight loss exceeding 5% of pre‑pregnancy weight.
- Severe dehydration signs: dizziness, dark urine, rapid heartbeat.
If any of these occur, seek medical care promptly. Early intervention can protect both you and your baby.
Frequently Asked Questions
Is it safe to take ginger supplements every day?
Yes, most studies show that up to 1gram of ginger per day is safe during pregnancy. Stick to the recommended dose and avoid excessive amounts that could cause heartburn.
Can I use over‑the‑counter antacids for nausea?
Some antacids (like Tums) can neutralize stomach acid and temporarily ease nausea, but they don’t treat the underlying hormonal cause. They’re fine for occasional use but shouldn’t replace vitaminB6 or ginger.
Why does morning sickness often improve after the first trimester?
Hormone levels, especially hCG, peak around weeks8‑12 and then level off. As the body adapts, the stomach’s sensitivity usually diminishes, easing nausea for most women.
Are there any foods I should avoid completely?
Fatty, fried, or heavily spiced foods often trigger nausea. Also, strong‑smelling items like garlic, onions, and certain cheeses can be problematic for many pregnant people.
How can I tell the difference between normal nausea and hyperemesis gravidarum?
Hyperemesis gravidarum is a severe form of vomiting that leads to weight loss, dehydration, and electrolyte imbalance. If you’re losing weight or can’t keep any fluids down, get medical attention right away.

Patrick Renneker
October 10, 2025 AT 14:57While the prevailing wisdom extols ginger and vitamin B6 as panaceas for pregnancy‑related nausea, a more discerning examination reveals a paucity of unequivocal evidence. The cited studies often suffer from small sample sizes and heterogeneous dosing regimens, which dilute their statistical power. Moreover, the mechanistic rationale-that ginger accelerates gastric emptying-remains speculative at best. One must also consider the potential for gastrointestinal irritation when ingesting concentrated ginger extracts on an empty stomach. Vitamin B6, although generally regarded as safe, can precipitate neuropathic symptoms in susceptible individuals when consumed beyond recommended limits. The recommendation to ingest 25‑50 mg thrice daily tacitly assumes uniform metabolic capacity across the pregnant population, an assumption lacking empirical support. In addition, the emphasis on small, frequent meals disregards the cultural and socioeconomic realities that shape dietary patterns. For many, the logistics of preparing multiple snacks per day constitute an untenable burden. Acupressure wristbands, frequently lauded for their efficacy, have demonstrated, in rigorous double‑blind trials, only a marginal reduction in nausea scores compared with sham devices. The placebo effect, a potent confounder, may account for much of the perceived benefit. Hydration strategies, such as electrolyte beverages, while intuitively sound, have not been conclusively linked to reduced emesis frequency in controlled studies. Consequently, the indiscriminate endorsement of these modalities may engender a false sense of control while diverting attention from clinically validated interventions. It is incumbent upon clinicians to appraise each recommendation through a lens of individualized risk‑benefit analysis. Patients should be encouraged to maintain a symptom diary, not merely to inform their own self‑management but also to furnish their providers with actionable data. In sum, the heterogeneity of the evidence base warrants a cautious, personalized approach rather than a one‑size‑fits‑all prescription.
KAYLEE MCDONALD
October 23, 2025 AT 08:30Totally get how exhausting morning sickness can be-keep those crackers within arm’s reach and sip ginger tea before you even get out of bed.
Alec McCoy
November 5, 2025 AT 01:03Hey there, you’re not alone in this roller‑coaster-most expectant folks wrestle with nausea during the first trimester. Start by establishing a “snack station” on your nightstand: plain crackers, a banana, or a small yogurt. Pair those carbs with a protein source like a dab of peanut butter to keep blood sugar steady. Hydration is key; sip water or an electrolyte drink slowly every hour rather than gulping. If ginger is tolerable, try a few candied slices or a warm ginger tea before meals. Vitamin B6 supplements can be useful, but check the dosage with your OB‑GYN first. Acupressure bands are worth a shot-just wear them consistently. And remember, tracking your symptoms in a simple notebook can reveal patterns you might otherwise miss.
Aaron Perez
November 17, 2025 AT 18:37One might contemplate the ontological underpinnings of nausea, yet, paradoxically, the corporeal manifestation persists-an undeniable reminder that philosophy does not quell gastric reflux; nevertheless, the experiential reality remains, undeniably, a potent disruptor of quotidian equilibrium. In the grand tapestry of human physiology, the surge of hormonal flux is not merely a biochemical fact, but a narrative that challenges our epistemic frameworks; consequently, it demands both introspection and empirical scrutiny. While some cling to anecdotal remedies as if they were axiomatic truths, the prudent skeptic will demand rigorous, double‑blind validation before bestowing universal credence. Ultimately, the interplay between mind and gut underscores a profound dialectic, urging us to reconcile metaphysical speculation with the palpable sensations of the belly.
William Mack
November 30, 2025 AT 12:10Avoid strong odors and keep a ginger stash handy.
Julia C
December 13, 2025 AT 05:43Honestly, this whole “chew on ginger” hype feels like a marketing ploy.
John Blas
December 25, 2025 AT 23:17Ugh, another post about “tips” when I’m literally losing weight every day-this is beyond frustrating.
Darin Borisov
January 7, 2026 AT 16:50Permit me, if you will, to articulate a nuanced perspective on the purported efficacy of “geriatric ginger” regimens; while the phytochemical constituents-gingerol, shogaol, and their kin-exhibit demonstrable anti‑emetic properties in vitro, the translational leap to clinical praxis is beset by dosage heterogeneity and patient-specific pharmacodynamics. Moreover, the psychosomatic overlay-wherein expectancy effects potentiate symptomatic relief-cannot be discounted as a mere epiphenomenon. In practice, I advocate a stratified protocol: initiate with 250 mg of standardized ginger extract three times daily, monitor for both therapeutic benefit and gastrointestinal tolerance, and, contingent upon satisfactory response, integrate a calibrated vitamin B6 supplement calibrated at 10‑20 mg per dose. Concomitantly, the deployment of P6 acupressure bands should be framed not as a panacea, but as an adjunctive modality, employed in concert with optimal dietary spacing-ideally a 2–3‑hour interval between low‑glycemic carbohydrate boluses. It is incumbent upon clinicians to eschew dogmatic prescription in favor of an evidence‑informed, patient‑centric algorithm, thereby mitigating the risk of iatrogenic overreach while honoring the empirical footprint of centuries‑old herbal wisdom.
Sean Kemmis
January 20, 2026 AT 10:23Data shows no clear benefit.
Nathan Squire
February 2, 2026 AT 03:57Oh, absolutely, because nothing says "I trust my doctor" like a sarcastic note tucked into a forum comment. If you’ve already tried every home remedy under the sun and still feel like you’re auditioning for an amateur vomiting contest, then by all means, keep scrolling for the next miracle: a unicorn‑infused smoothie. In reality, the best strategy remains the boring, mundane one-consult your obstetrician, follow a balanced diet, and stay hydrated. Any flashy hack that promises instant relief without medical oversight is, frankly, a recipe for disappointment.
satish kumar
February 14, 2026 AT 21:30While the conventional narrative extols ginger, vitamin B6, and acupressure as universally applicable remedies, one must, with a judicious eye, interrogate the underlying assumptions, question the homogeneity of study populations, and consider the myriad cultural, physiological, and psychosocial variables that render a one‑size‑fits‑all prescription not only implausible, but potentially detrimental; consequently, a more discerning approach, predicated upon individualized assessment, incremental experimentation, and vigilant monitoring, emerges as the prudent pathway forward.
Matthew Marshall
February 27, 2026 AT 15:03And just when you think you’ve mastered the morning tide, your stomach erupts like a volcanic surprise.