Hypertensive Retinopathy: How High Blood Pressure Damages Your Eyes
 Nov, 22 2025
Nov, 22 2025
Most people know that high blood pressure can lead to heart attacks or strokes. But fewer realize it can also silently destroy your vision-long before you notice any symptoms. Hypertensive retinopathy isn’t a rare complication. It’s a direct result of uncontrolled hypertension, and it’s happening to millions of Americans right now. The damage starts in the tiny blood vessels at the back of your eye. If left unchecked, it can lead to permanent vision loss. The good news? You can catch it early-and stop it in its tracks.
What Happens Inside Your Eye When Blood Pressure Stays Too High
Your retina is like the film in a camera. It captures light and sends images to your brain. But it’s also packed with delicate blood vessels, no thicker than a human hair. When your blood pressure stays high, these vessels get squeezed, stretched, and damaged over time. The walls thicken. Blood flow slows. Leaks happen. This isn’t just a theory-it’s visible through an eye exam. The changes follow a clear pattern, first mapped out in the 1930s by Keith, Wagener, and Barker. Today, doctors still use their system-called the KWB classification-to grade how bad the damage is. Grade 1 might look like mild narrowing of arteries. By Grade 4, you’re looking at swelling of the optic nerve, bleeding, and fluid buildup. That’s when vision loss becomes likely. Studies show that even at blood pressure levels of 140/90 mmHg-classified as Stage 1 hypertension-retinal changes can appear after just three years. And if your systolic pressure climbs above 160 mmHg for more than five years, the risk of permanent damage jumps sharply. The retina doesn’t lie. It’s one of the few places in your body where doctors can actually see what high blood pressure is doing to your blood vessels in real time.The Warning Signs You Can’t Ignore
Here’s the scary part: you might not feel a thing. In fact, 68% of people with early-stage hypertensive retinopathy have no symptoms at all. That’s why routine eye exams are just as important as checking your blood pressure at home. When symptoms do show up, they’re often mistaken for something else. Blurry vision? Maybe you just need new glasses. Dark spots in your central vision? Oh, you’re just tired. But if you’re over 40 and have high blood pressure, these aren’t normal. In advanced cases, patients describe a “curtain” coming down over part of their vision-like a shade being pulled across their eyes. Some report sudden double vision or severe headaches along with it. These aren’t coincidences. They’re red flags. One patient in a Reddit thread described waking up with dark spots after his blood pressure spiked to 210/110. Another mentioned losing 40% of his peripheral vision overnight. These aren’t rare stories. Clinical data shows that 85% of people with Grade 3 or 4 retinopathy experience noticeable vision problems. And 27% report sudden vision loss during a hypertensive crisis. If you’re experiencing any of these, don’t wait. Go to an eye doctor immediately.How Doctors Diagnose Retinal Damage
Your eye doctor doesn’t need fancy equipment to spot early signs. A simple fundoscopic exam-where they shine a light into your eye and look at the retina-can reveal narrowing arteries, hemorrhages, or cotton wool spots (tiny white patches caused by blocked blood flow). But modern tools are making detection faster and more accurate. Optical coherence tomography (OCT) scans can measure swelling in the retina down to the micrometer. AI-powered imaging systems like IDx-DR and RetinaCheck AI are now cleared by the FDA to analyze retinal photos and flag signs of hypertensive damage with 92% accuracy-up from 75% just a few years ago. These tools are being rolled out in primary care offices, not just eye clinics, making early detection more common. The key is timing. Ophthalmologists can detect changes at blood pressure levels as low as 140/90 mmHg. That’s why the American Heart Association now recommends annual eye exams for anyone with hypertension-and every six months for those with resistant hypertension (blood pressure that won’t drop even after taking three medications).
What the Stages Really Mean
Understanding the KWB stages isn’t just medical jargon. It tells you how urgent your situation is.- Grade 1: Mild narrowing of arteries. No bleeding or leakage. Often asymptomatic. Still, this is your body’s first warning.
- Grade 2: Arteriovenous nicking-where arteries press down on veins, pinching them. Blood flow is restricted. This stage increases your stroke risk by 3.2 times.
- Grade 3: Now you see hemorrhages (flame-shaped or dot-like), hard exudates (yellow lipid deposits), and cotton wool spots. Vision may start to blur. This stage means your retina is leaking fluid and lipids. Damage is becoming structural.
- Grade 4: Swelling of the optic nerve (papilledema). This is a medical emergency. It means your brain is under pressure too. About 78% of patients at this stage have other organ damage-heart, kidneys, or brain. Many will have a stroke within a year if blood pressure isn’t brought down.
Can You Reverse the Damage?
The answer depends on how far it’s gone. If caught early-Grade 1 or 2-strict blood pressure control can stop progression and even reverse some changes. Studies show that lowering systolic pressure by 25 mmHg within 48 hours resolves acute retinal swelling in 65% of cases. Vision improvement often begins within a week. But if you’ve reached Grade 3 or 4, the damage is harder to undo. Fluid leaks can scar the macula-the part of the retina responsible for sharp central vision. Once that’s damaged, recovery is partial at best. About 22% of patients with advanced retinopathy end up with permanent visual field defects, even after their blood pressure is perfectly managed. The key isn’t just lowering your numbers. It’s doing it consistently. People who check their blood pressure at home and stick to their meds have 70% better adherence than those who don’t. And those who link their eye health to their blood pressure management are 35% more likely to keep their numbers in range, according to the American Heart Association’s “Check. Change. Control.” program.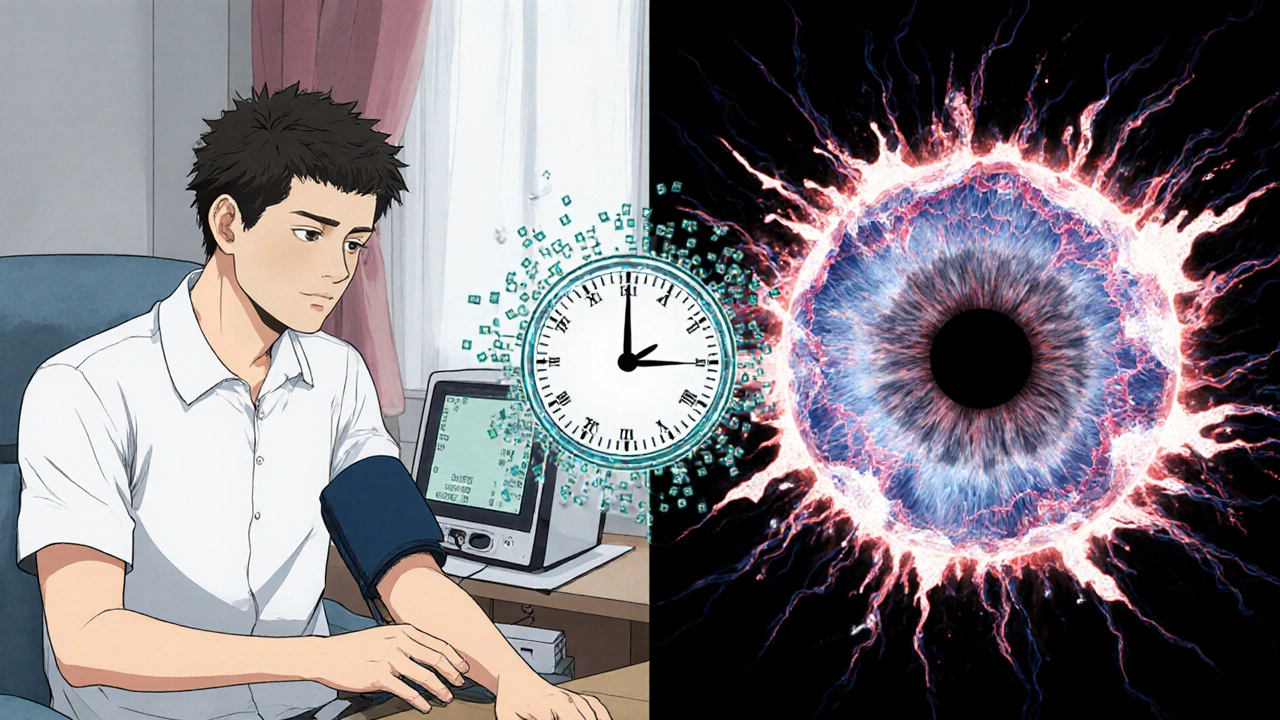
What You Can Do Right Now
You don’t need to wait for symptoms. If you have high blood pressure, here’s what to do:- Get a dilated eye exam. Even if you have 20/20 vision. If you’re over 40 and have hypertension, make this a yearly checkup. If your BP is hard to control, do it every six months.
- Track your blood pressure at home. Buy a validated monitor. Take readings twice a day, at the same times. Write them down. Bring them to your doctor.
- Know your numbers. Systolic over 140 or diastolic over 90? That’s Stage 1. Over 160/100? That’s Stage 2. Both put you at risk.
- Don’t ignore eye changes. Blurry vision, dark spots, sudden vision loss-these aren’t normal. Call your eye doctor immediately.
- Ask about medications. Some blood pressure drugs, like ACE inhibitors, have been shown to reduce retinal damage progression by 32% compared to others. Talk to your doctor about the best option for your eyes and your heart.
The Bigger Picture: Your Eyes Are a Mirror
Hypertensive retinopathy isn’t just about your vision. It’s a warning sign that your entire vascular system is under siege. People with retinal damage have a 2.5 times higher risk of heart attack and stroke. The same vessels that are leaking in your eye are likely stiffening in your brain, kidneys, and heart. That’s why the National Eye Institute calls the retina a “window to systemic vascular health.” What you see in your eye tells you what’s happening inside your body. And if you’re ignoring your eyes because you “feel fine,” you’re ignoring the most honest indicator you’ve got. The good news? You’re not powerless. With early detection and consistent management, 85% of early-stage cases stabilize without further damage. The difference between keeping your vision and losing it often comes down to one thing: whether you got your eyes checked before you started having symptoms.Can hypertensive retinopathy cause blindness?
Yes, if left untreated. Advanced stages-especially Grade 3 and 4-can lead to permanent vision loss through scarring of the macula, optic nerve damage, or retinal detachment. While not everyone with high blood pressure goes blind, the risk increases sharply after five years of uncontrolled hypertension. Early detection and treatment can prevent this.
Do I need an eye exam if I have high blood pressure but no vision problems?
Absolutely. Up to 68% of people with early-stage hypertensive retinopathy have no symptoms at all. Damage can be happening without you knowing. Annual dilated eye exams are recommended for anyone with hypertension, especially if your blood pressure is above 140/90 mmHg.
How long does it take for high blood pressure to damage the retina?
Signs can appear in as little as three years with uncontrolled hypertension. The longer your blood pressure stays high, the greater the damage. Studies show that after five years of systolic pressure over 160 mmHg, the risk of retinal changes increases dramatically. Even mild hypertension (130-139 mmHg) can cause damage if it lasts 10 years or more.
Can lifestyle changes reverse hypertensive retinopathy?
Lifestyle changes-like reducing salt, losing weight, exercising, and quitting smoking-are critical for lowering blood pressure. When combined with medication, they can stop progression and even reverse early damage. But once there’s bleeding, scarring, or optic nerve swelling, lifestyle changes alone won’t fix it. Medical treatment is required.
Are there new technologies for detecting hypertensive retinopathy?
Yes. AI-powered retinal imaging tools like RetinaCheck AI and IDx-DR are now FDA-cleared and used in clinics nationwide. They analyze digital retinal photos and detect signs of damage with 92% accuracy-better than many human doctors. Non-invasive devices like RetiFlow, which measures capillary blood flow, are also in advanced trials and may soon allow for real-time monitoring without dyes or scans.
Does having diabetes make hypertensive retinopathy worse?
Yes, significantly. People with both diabetes and hypertension have a 4.7 times higher risk of permanent vision loss than those with just one condition. The damage from diabetic retinopathy and hypertensive retinopathy can overlap and accelerate each other. Managing both conditions aggressively is essential to protect your vision.

Amy Hutchinson
November 23, 2025 AT 07:42Archana Jha
November 23, 2025 AT 09:23Aki Jones
November 24, 2025 AT 18:22Jefriady Dahri
November 25, 2025 AT 22:09Sharley Agarwal
November 27, 2025 AT 16:43Shivam Goel
November 29, 2025 AT 09:51Leisha Haynes
November 29, 2025 AT 13:42Kimberley Chronicle
November 29, 2025 AT 14:58Shirou Spade
December 1, 2025 AT 00:19Lisa Odence
December 1, 2025 AT 16:20Dolapo Eniola
December 1, 2025 AT 17:52giselle kate
December 2, 2025 AT 09:09Emily Craig
December 2, 2025 AT 12:39Karen Willie
December 3, 2025 AT 23:51Jennifer Griffith
December 5, 2025 AT 00:41Roscoe Howard
December 6, 2025 AT 08:39Patricia McElhinney
December 7, 2025 AT 14:51Agastya Shukla
December 8, 2025 AT 22:08Pallab Dasgupta
December 9, 2025 AT 02:34Ellen Sales
December 11, 2025 AT 01:07