Fibromyalgia: How Widespread Pain Is Treated with Antidepressants
 Nov, 21 2025
Nov, 21 2025
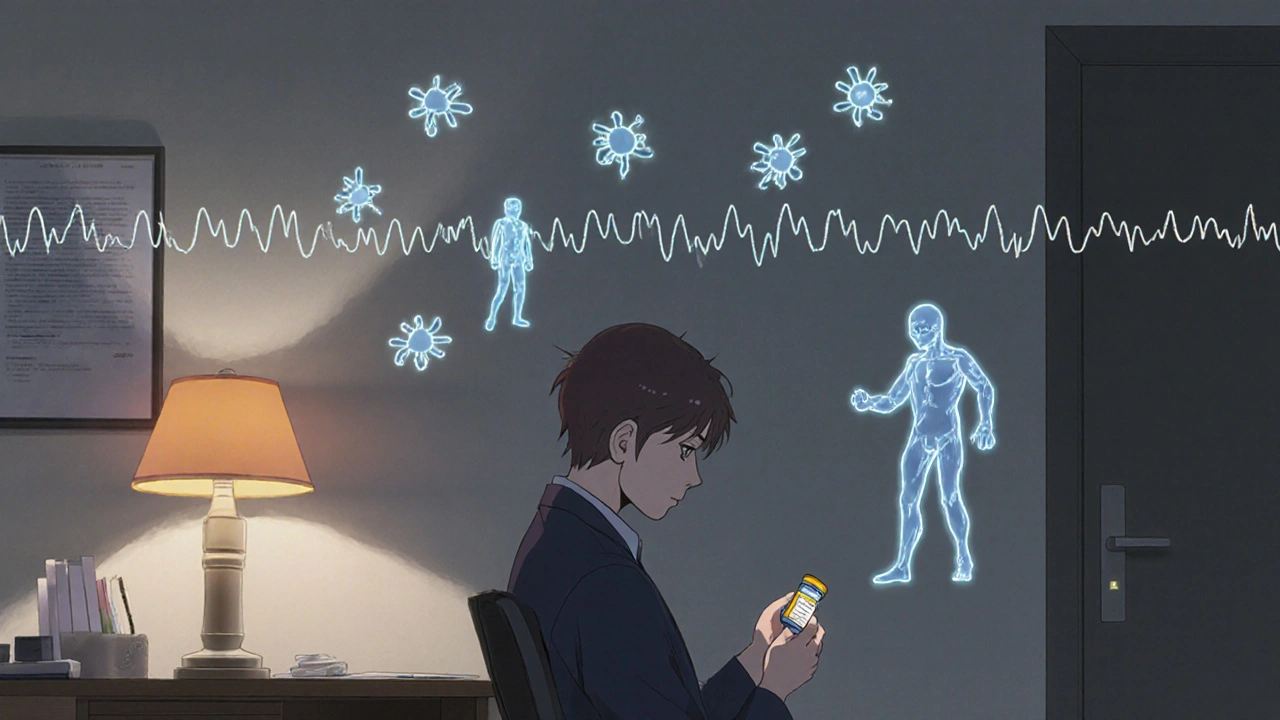
For millions of people, waking up with body-wide aches that don’t go away isn’t just bad luck-it’s daily life. Fibromyalgia isn’t a muscle strain, not arthritis, and not in your head. It’s a real, measurable condition where the nervous system turns up the volume on pain signals, making even light touches feel overwhelming. The pain isn’t localized; it’s widespread, lasting at least three months, and comes with crushing fatigue, brain fog, and sleep so broken you wake up more tired than when you lay down. If you’ve been told it’s "all in your mind," you’re not alone-but science now confirms this is a neurological issue, not a psychological one.
What Fibromyalgia Really Is
Fibromyalgia affects 2 to 8% of people worldwide, and women make up 75 to 90% of diagnosed cases. It’s not caused by injury or inflammation. Instead, the brain and spinal cord become hypersensitive. Pain signals that should be mild get amplified. That’s why pressing on a tender spot hurts, but a hug can feel unbearable. The American College of Rheumatology updated its diagnostic criteria in 2016 to focus less on pressure points and more on symptom patterns: widespread pain plus at least four other symptoms like poor sleep, memory trouble, or feeling drained all day.
There’s no blood test. No X-ray shows it. That’s why diagnosis often takes years-on average, five. Many patients see six or more doctors before someone listens. But the lack of a lab marker doesn’t make it less real. Think of it like migraines: no scan proves them, yet they’re debilitating. Fibromyalgia is the same. The pain is physical, even if the source is in the nervous system.
Why Antidepressants Are Used for Pain
It sounds confusing: why give someone depression medicine for pain? The answer isn’t about mood. Antidepressants like duloxetine and amitriptyline work on brain chemicals-serotonin and norepinephrine-that also control how pain signals travel. In fibromyalgia, these chemicals are out of balance. Boosting them helps calm the overactive pain system.
Three drugs are FDA-approved specifically for fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella), and pregabalin (Lyrica). Two of them-duloxetine and milnacipran-are SNRIs, a class of antidepressants. Pregabalin isn’t an antidepressant, but it works on the same nerve pathways. Amitriptyline, an older tricyclic antidepressant, isn’t FDA-approved for fibromyalgia but is prescribed off-label because it’s cheap, effective for sleep, and helps with pain.
Studies show these drugs reduce pain by 20 to 30% in about half the people who take them. That might not sound like much, but for someone who’s been in constant pain for years, even a 25% drop means you can get out of bed, take a shower, or play with your kids without crying. The key is managing expectations: these aren’t magic pills. They’re tools to help you rebuild your life.
How Antidepressants Actually Work in Fibromyalgia
When you start an antidepressant for fibromyalgia, you’re not trying to fix depression-you’re trying to quiet a nervous system that’s screaming. These drugs don’t work like painkillers. They don’t numb the area. Instead, they change how your brain interprets signals from your body.
For example, duloxetine starts at 30 mg a day, sometimes even 20 mg, to avoid side effects. It takes 4 to 6 weeks to kick in. You might feel more tired at first, or nauseous. That’s normal. The goal isn’t to feel euphoric. It’s to feel less overwhelmed by pain. Many patients report better sleep within two weeks, even before pain improves. That’s because these drugs help regulate sleep cycles, which are often shattered in fibromyalgia.
Amitriptyline, taken at night, works differently. At low doses (10 to 25 mg), it doesn’t lift mood-it just helps you sleep deeper. And better sleep means less pain sensitivity the next day. One patient on MyFibroTeam said, “After 10 years of insomnia, 10 mg of amitriptyline finally let me sleep through the night.” That’s not a miracle. It’s science.
But side effects are real. Dry mouth, dizziness, weight gain, and drowsiness are common. About 25 to 30% of people quit because they can’t tolerate them. That’s why doctors now start low and go slow. A 5 mg dose of amitriptyline at bedtime, slowly increased by 5 mg every week, is far better tolerated than jumping to 50 mg.
Antidepressants vs. Exercise: What Actually Works Best
Here’s the hard truth: exercise beats medication for long-term results. Not just walking. Not just stretching. But consistent, low-impact movement-like tai chi, yoga, or water aerobics.
A 2022 Arthritis Foundation study found that people who did tai chi for 12 weeks reduced their pain by 20 to 30%. Yoga cut pain intensity by 24%. And those benefits kept growing. After six months, 70% of people who stuck with exercise saw 25 to 35% less pain. That’s better than most drugs.
Antidepressants? They help about 50% of people, but the effect fades after 6 to 12 months. Side effects pile up. Many stop taking them. But exercise? The more you do, the better your body gets at handling pain. Your muscles strengthen. Your nerves calm down. Your sleep improves. It’s a feedback loop of healing.
That’s why experts like Dr. Daniel Clauw at the University of Michigan call exercise the “single most effective treatment”-and the most underused. Most patients are handed a pill before they’re told to move. That’s backwards.
The Best Approach: Combine Them
The smartest strategy isn’t choosing between pills and movement. It’s using both.
Start with exercise-but start small. Ten minutes a day, three times a week. If you flare up, back off. Don’t push through pain. Use the “10% rule”: increase activity by no more than 10% each week. Add tai chi or yoga. These aren’t just workouts-they’re mindfulness practices that retrain your nervous system.
Then, if pain is still crippling, add a low-dose antidepressant. A 20 mg dose of duloxetine, or 10 mg of amitriptyline at night. Don’t expect overnight results. Wait 4 to 8 weeks. Track your sleep, pain levels, and energy. If it helps, keep going. If side effects are worse than the pain, talk to your doctor about lowering the dose or switching.
One patient on PatientsLikeMe combined 20 mg of duloxetine with tai chi three times a week. She said, “I finally feel like I’m not drowning.” That’s the goal-not to be pain-free, but to be in control.

What Doesn’t Work-and Why
Don’t waste time on opioids. The CDC explicitly warns against them for fibromyalgia. They don’t work on nerve pain and carry a high risk of addiction. Steroids? Useless. Anti-inflammatories like ibuprofen? Mostly ineffective because fibromyalgia isn’t inflamed tissue-it’s a misfiring nervous system.
Acupuncture can help some people-about 15 to 25% pain reduction-but it requires weekly sessions for months. It’s not a quick fix. Same with CBD: some swear by it, but solid evidence is still lacking. Stick with what’s been studied: movement, therapy, and carefully chosen meds.
And don’t let anyone tell you it’s “all in your head.” The brain changes in fibromyalgia are visible on fMRI scans. Your pain is real. You’re not weak. You’re not lazy. You’re dealing with a complex neurological condition-and you’re not alone.
Where to Start Today
If you’ve just been diagnosed:
- Get educated. Use the CDC’s free online course, “Managing Fibromyalgia.”
- Start moving. Walk 10 minutes a day. Add a YouTube yoga or tai chi video three times a week.
- Track your symptoms. Use a simple journal: rate pain (1-10), sleep (1-10), energy (1-10) daily.
- Ask your doctor about starting a low-dose antidepressant if pain is above 7/10 and sleep is broken.
- Find a support group. The Fibromyalgia Support Group on Reddit has over 100,000 members sharing real tips.
Don’t wait for a cure. There isn’t one yet. But there are tools. And with the right mix, most people can live full, meaningful lives-even with chronic pain.
Are antidepressants the first treatment for fibromyalgia?
No. Current guidelines from the American College of Rheumatology and the American Academy of Family Physicians say exercise, cognitive behavioral therapy, and education should come first. Antidepressants are added only if pain and fatigue remain severe after trying non-drug options. They’re not a starting point-they’re a support tool.
How long does it take for antidepressants to work for fibromyalgia pain?
It usually takes 4 to 6 weeks to feel any pain relief from SNRIs like duloxetine or milnacipran. Amitriptyline may help sleep in 2 to 4 weeks, but pain reduction often takes 6 to 8 weeks. Patience is key. Don’t stop too soon. If there’s no improvement after 10 to 12 weeks, talk to your doctor about adjusting or switching.
Can I stop taking antidepressants once I feel better?
Not without talking to your doctor. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or brain zaps. Even if you feel better, keep taking the medication for at least 6 months. Then, if your pain is well-managed and you’re exercising regularly, your doctor may help you taper off slowly. Many people stay on low doses long-term because they help with sleep and pain control.
Why do some people say antidepressants made their pain worse?
Side effects can mimic or worsen symptoms. Duloxetine, for example, can cause increased anxiety, nausea, or dizziness-especially at higher doses. Some people mistake these side effects for their fibromyalgia flaring. Starting too high (like 60 mg right away) increases this risk. That’s why doctors now recommend starting at 20 or 30 mg and increasing slowly. If you feel worse, don’t ignore it-talk to your provider. Lowering the dose often helps.
Is there a new treatment coming for fibromyalgia?
Yes. In February 2024, the FDA accepted a new drug application for centanafadine (XRS-001), which showed 35% pain reduction in clinical trials with fewer side effects than current options. It’s not available yet, but if approved, it could become a major option by late 2025 or 2026. Other research is exploring brain stimulation devices and blood tests to identify fibromyalgia subtypes for personalized treatment.

John Mackaill
November 23, 2025 AT 00:48I’ve been on amitriptyline for 18 months now-10mg at night. Didn’t fix everything, but I finally sleep through the night. No more 3am panic spirals. That alone made it worth it. I still do yoga three times a week. Pills don’t cure, but they buy you space to heal.
Adrian Rios
November 23, 2025 AT 11:08Let me tell you something that no one talks about: the real magic isn’t the drug-it’s the routine. You take the pill, sure, but what actually changes your life is showing up for yourself every day-even if it’s just five minutes of stretching. I used to think fibromyalgia was a death sentence. Now? I wake up, drink my tea, roll out my mat, and remind myself that pain doesn’t own me. The medication helped me get to that point. But movement? Movement gave me back my dignity. And that’s worth more than any prescription.
Casper van Hoof
November 25, 2025 AT 01:43It is, in fact, a fascinating neurophysiological phenomenon that the central nervous system, in the absence of peripheral tissue damage, can sustain a state of hyperalgesia and allodynia-conditions that are demonstrably measurable via quantitative sensory testing and functional neuroimaging. The pharmacological modulation of serotonergic and noradrenergic pathways represents a rational, albeit imperfect, therapeutic strategy grounded in descending pain inhibition theory. One might argue, however, that the emphasis on pharmacological intervention risks pathologizing chronic pain as a biochemical deficit, rather than a complex biopsychosocial adaptation.
Richard Wöhrl
November 25, 2025 AT 07:22Just want to say-this post is spot-on. I’ve been through the 6-doctor, 5-year diagnostic nightmare. And yes, the lack of a blood test makes people doubt you. But fMRI scans show real differences in brain activity. I started with 20mg duloxetine. First two weeks? Nausea, dizziness, felt like I was drowning. But by week 5? I slept 6 hours straight for the first time in years. Then I added 10-minute walks. Then yoga. Now? I’m not pain-free-but I’m functional. And that’s the goal. Don’t let anyone tell you that low-dose meds are ‘just placebo.’ They’re not. They’re neuro-modulators. And they work-if you give them time, and pair them with movement. Seriously. Try the 10% rule. It’s life-changing.
Pramod Kumar
November 26, 2025 AT 17:16Man, this hits different. I remember crying in a doctor’s office because I couldn’t lift my coffee cup. They gave me ibuprofen. Like that was gonna fix a screaming nervous system. Then I found tai chi-slow, gentle, like water moving through stone. And amitriptyline, 15mg at night. Not for mood. For sleep. For quiet. Now I wake up and feel… human. Not broken. Just healing. To everyone out there: you’re not lazy. You’re not weak. Your body’s just been hijacked. And you’re still fighting. That’s courage.
Brandy Walley
November 27, 2025 AT 13:21shreyas yashas
November 28, 2025 AT 07:03Brandy’s comment made me chuckle. Dude, if you’re on three jobs and can’t move? I get it. But even 2 minutes of deep breathing counts. I work in a call center, 12-hour shifts, chronic pain. I do seated leg lifts between calls. 10 reps. That’s it. And I take 10mg amitriptyline. Not because I’m depressed. Because my nerves are on fire. You don’t need a gym. You just need to start small. And stop listening to people who think pain is a choice.
Suresh Ramaiyan
November 29, 2025 AT 08:17There’s a quiet rebellion in showing up for yourself when your body feels like a traitor. You don’t need to be ‘fixed.’ You just need to be heard. The antidepressants? They’re not magic. But they’re a bridge. And movement? That’s the path. I used to think I had to choose between pills and yoga. Now I see it’s not either/or-it’s both. Like using a crutch while rebuilding your leg. One holds you up. The other makes you strong. And if you’re tired? That’s okay. Rest is part of the process too. You’re not failing. You’re adapting.
Katy Bell
November 30, 2025 AT 18:48I started with 30mg duloxetine. Thought I was going to die from the side effects. But I stuck with it. And I started walking around my apartment for 7 minutes every morning. Just… walking. No music. No podcast. Just me and my breath. After 6 weeks? I cried because I picked up my daughter without wincing. That’s the win. Not the pill. Not the yoga. That moment. The quiet, stupid, beautiful moment where pain didn’t win. And yeah-I still have bad days. But now I know I can survive them.
Lisa Lee
December 2, 2025 AT 13:18