Bleeding Risk from SSRIs: How Platelet Dysfunction Increases Bleeding Danger
 Jan, 14 2026
Jan, 14 2026
SSRI Bleeding Risk Calculator
This calculator estimates your bleeding risk based on your SSRI medication, age, and other risk factors. It's designed for informational purposes only and shouldn't replace professional medical advice.
Your SSRI Selection
Age & Health Factors
Medication Factors
When you take an SSRI for depression or anxiety, you’re not just changing your mood-you’re also affecting how your blood clots. It’s not something most people think about, but the same mechanism that helps lift your spirits can quietly increase your risk of bleeding. This isn’t a rare side effect. It’s a well-documented, biologically grounded risk that shows up in hospitals, emergency rooms, and even in everyday bruises that won’t go away.
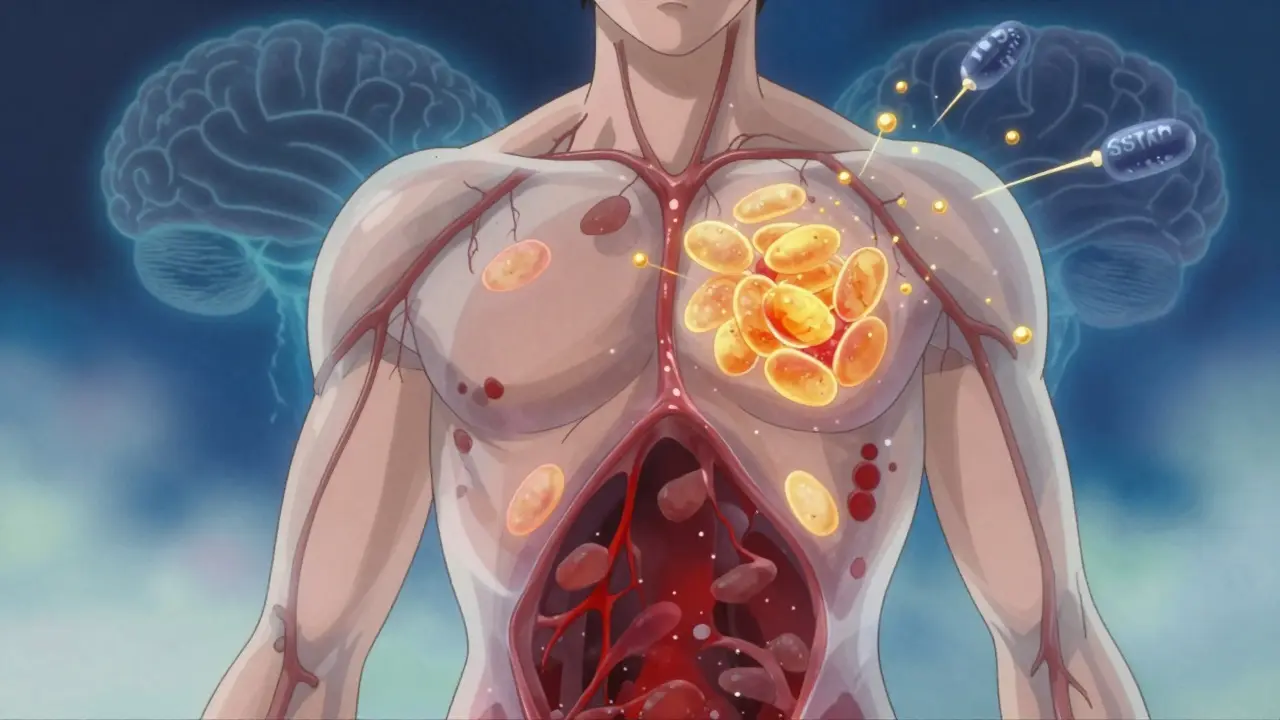
How SSRIs Interfere with Platelets
SSRIs like sertraline, fluoxetine, and paroxetine work by blocking the serotonin transporter, which normally pulls serotonin back into brain cells after it’s released. More serotonin in the brain helps ease depression. But here’s the catch: 99% of your body’s serotonin isn’t in your brain. It’s in your platelets.
Platelets are the tiny blood cells that rush to a cut and stick together to form a clot. They need serotonin to do their job properly. When serotonin is released at the site of injury, it acts like a signal to recruit more platelets. Without enough serotonin inside them, platelets become sluggish. They don’t clump together as quickly or as strongly. Studies show that people on paroxetine can lose over 80% of their platelet serotonin. That’s not a small drop-it’s a major disruption to your body’s natural stop-the-bleeding system.
This isn’t theory. Lab tests confirm it. When doctors test platelet function in people taking SSRIs, they see reduced aggregation. The more the drug blocks serotonin uptake, the worse the effect. Paroxetine and fluvoxamine are the strongest inhibitors, so they hit platelets the hardest. Sertraline and citalopram? They’re milder. That’s why bleeding risk isn’t the same across all SSRIs.
Who’s Most at Risk?
Not everyone on SSRIs will bleed. But some people are sitting on a ticking clock. If you’re already taking blood thinners like warfarin, apixaban, or rivaroxaban, your risk jumps. A 2024 meta-analysis found that combining SSRIs with oral anticoagulants raises the chance of major bleeding by 35%. That’s not a tiny increase. It’s the difference between 3 in 100 and 4 in 100 people having a dangerous bleed over a year.
Other red flags? You’re over 65. You’ve had a stomach ulcer. You’re on NSAIDs like ibuprofen or naproxen. Those painkillers irritate your stomach lining and stop platelets from working too. Add an SSRI? The risk multiplies. One study showed NSAIDs combined with SSRIs increase bleeding risk by 4.5 times. That’s why doctors often tell patients to avoid these combinations.
People with kidney or liver disease are also more vulnerable. Their bodies clear drugs slower, so SSRIs build up. That means even a mild SSRI like sertraline can become a bigger problem over time. And if you’ve had bleeding before-whether it’s nosebleeds, heavy periods, or a GI bleed-you’re at higher risk of it happening again.
Which SSRIs Are Riskiest?
Not all SSRIs are created equal when it comes to bleeding. The key is how tightly they bind to the serotonin transporter. The tighter the grip, the more serotonin gets stripped from platelets.
Here’s how they stack up by binding strength:
- Paroxetine - Ki = 0.17 nM (highest risk)
- Fluvoxamine - Ki = 0.34 nM
- Fluoxetine - Ki = 0.45 nM
- Sertraline - Ki = 0.52 nM
- Citalopram - Ki = 0.91 nM (lowest risk among SSRIs)
Real-world data backs this up. In FDA reports from 2010-2020, paroxetine users were twice as likely to report gastrointestinal bleeding compared to those on sertraline. A Drugs.com survey of nearly 3,000 users found 18.7% of paroxetine users reported easy bruising. For sertraline? Just 9.2%. Reddit threads from SSRI users echo this: 74% of people who reported excessive bleeding were on paroxetine. Only 32% were on sertraline.
That’s why prescribing patterns are shifting. Since 2015, paroxetine prescriptions have dropped 37% in patients with stomach issues or bleeding history. Sertraline prescriptions have gone up by nearly 30% in the same group. Doctors aren’t avoiding SSRIs-they’re choosing the safer ones.

What About Surgery or Procedures?
If you’re scheduled for a tooth extraction, colonoscopy, or knee replacement, your doctor should know you’re on an SSRI. For minor procedures, the risk is low. But for surgeries with higher bleeding potential-like spinal surgery, liver resection, or cardiac bypass-the stakes are higher.
Here’s what experts recommend:
- For low-risk procedures: Keep taking your SSRI. Stopping can trigger depression relapse, which is dangerous in itself.
- For moderate-to-high-risk procedures: Consider stopping the SSRI 5-7 days before. This gives platelets time to rebuild their serotonin stores.
- For high-risk patients (HAS-BLED score ≥3): Avoid paroxetine and fluvoxamine. Use sertraline or citalopram instead.
- Never stop cold turkey. Always taper under medical supervision.
The American Psychiatric Association says: don’t stop SSRIs before cardiac surgery. The risk of depression triggering a heart attack outweighs the bleeding risk. But for other surgeries? Individualize. Ask your surgeon and psychiatrist to talk together.
What to Watch For
Most people on SSRIs never bleed. But you need to know the warning signs. If you notice any of these, don’t wait:
- Black, tarry stools (sign of upper GI bleeding)
- Vomiting blood or material that looks like coffee grounds
- Unexplained bruising-especially large patches or bruises without injury
- Nosebleeds that last longer than 10 minutes
- Heavy or prolonged menstrual bleeding
- Bleeding from gums that won’t stop after brushing
If you see any of these, call your doctor or go to urgent care. Don’t assume it’s ‘just a side effect.’
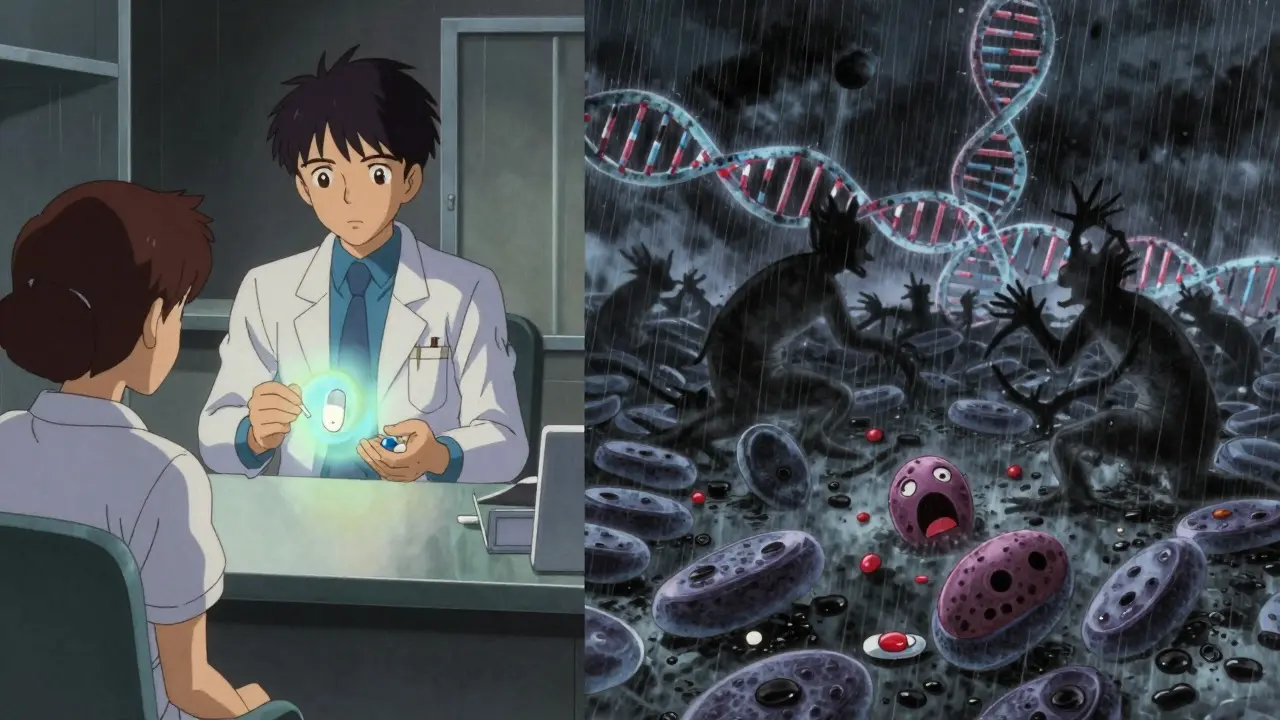
New Tools to Predict Risk
Doctors aren’t guessing anymore. Genetic testing is starting to help. A gene called 5-HTTLPR controls how many serotonin transporters you make. People with two short versions (S/S genotype) have fewer transporters. When they take an SSRI, their platelets lose serotonin even faster. A 2024 study found these people have 2.3 times higher bleeding risk than those with two long versions (L/L).
Right now, this test isn’t routine. But the European Medicines Agency is reviewing it for possible label updates by late 2025. In the future, your SSRI choice might be guided by your DNA.
There’s also experimental work on platelet-rich plasma infusions. One 2023 study gave this to SSRI patients before surgery and cut their bleeding time by over 40%. It’s not standard yet, but it shows we’re moving toward solutions, not just warnings.
What’s the Bottom Line?
SSRIs save lives. Untreated depression increases heart disease risk, suicide risk, and even death from other illnesses. You shouldn’t avoid them because of bleeding fears. But you should be smart about them.
Here’s what to do:
- If you’re on an SSRI and take blood thinners or NSAIDs-talk to your doctor. You may need to switch one.
- If you’re starting an SSRI and have a history of bleeding-ask for sertraline or citalopram, not paroxetine.
- If you’re scheduled for surgery-tell your surgeon you’re on an antidepressant. Don’t assume they know.
- If you notice unusual bruising or bleeding-don’t ignore it. It’s not normal.
The goal isn’t to stop SSRIs. It’s to use them safely. Your mental health matters. So does your physical safety. You don’t have to choose one over the other-you just need the right information.
Can SSRIs cause internal bleeding?
Yes. SSRIs can increase the risk of internal bleeding, especially in the gastrointestinal tract. Studies show a 20-50% higher risk of stomach or intestinal bleeding in SSRI users compared to non-users, particularly with paroxetine or when combined with NSAIDs or blood thinners. Signs include black, tarry stools, vomiting blood, or unexplained abdominal pain.
Is sertraline safer than paroxetine for bleeding risk?
Yes. Sertraline has a much weaker effect on the serotonin transporter than paroxetine. Clinical data shows paroxetine users have nearly double the risk of gastrointestinal bleeding compared to sertraline users. For patients with bleeding risk factors, sertraline or citalopram are preferred over paroxetine or fluvoxamine.
Should I stop my SSRI before a dental procedure?
Usually not. For simple procedures like fillings or cleanings, stopping your SSRI isn’t necessary. The bleeding risk is minimal. For more invasive procedures like extractions or gum surgery, your dentist may ask you to stop for 5-7 days-but only if you’re on a high-risk SSRI like paroxetine and have other bleeding risk factors. Never stop without talking to your prescriber.
Can I take ibuprofen with an SSRI?
It’s not recommended. Combining NSAIDs like ibuprofen or naproxen with SSRIs increases bleeding risk by 4.5 times. Both drugs affect platelets and the stomach lining. If you need pain relief, acetaminophen (Tylenol) is a safer choice. Always check with your doctor before mixing medications.
Do all SSRIs affect platelets the same way?
No. SSRIs vary widely in how strongly they block serotonin reuptake. Paroxetine and fluvoxamine are the strongest, leading to the highest bleeding risk. Sertraline and citalopram are weaker inhibitors and carry lower risk. Fluoxetine is moderate. Your doctor can choose based on your personal risk profile.
Does stopping an SSRI reduce bleeding risk?
Yes, but slowly. Platelet serotonin levels start to recover within 5-7 days after stopping an SSRI. Full recovery takes about 2 weeks. However, stopping abruptly can trigger withdrawal symptoms or depression relapse. Always taper under medical supervision. The benefit of reduced bleeding risk must be weighed against the risk of mental health deterioration.

shiv singh
January 15, 2026 AT 09:19Robert Way
January 15, 2026 AT 20:25Sarah Triphahn
January 16, 2026 AT 09:10Vicky Zhang
January 16, 2026 AT 11:29Allison Deming
January 17, 2026 AT 08:47Susie Deer
January 18, 2026 AT 09:59TooAfraid ToSay
January 19, 2026 AT 18:02Dylan Livingston
January 20, 2026 AT 12:23Andrew Freeman
January 20, 2026 AT 17:16says haze
January 21, 2026 AT 19:38Alvin Bregman
January 22, 2026 AT 16:03Sarah -Jane Vincent
January 23, 2026 AT 01:01Henry Sy
January 23, 2026 AT 06:16Anna Hunger
January 24, 2026 AT 06:58